
Santéch has been positioned as a Major Player in IDC MarketScape: U.S. Provider Data Management 2022 Vendor Assessment (doc #US48815718, Feb 2022).

Santéch has been positioned as a Major Player in IDC MarketScape*: U.S. Provider Data Management 2018 Vendor Assessment (doc #US44514018, December 2018).

Santech has been recognized by Gartner as Cool Vendor in 'Health-Value Management for U.S. Healthcare Payors 2017' by Bryan Cole, Jeff Cribbs and Brad Holmes.
Provider Network management is the complex, varied and regular set of activities that are collectively required to keep the network - every health plan's core asset - functioning at the highest point of productivity.
An Agile network accomplishes the following things:
- Superior member experience & access to care
- Contained medical cost
- Superior Provider experience
- Regulatory compliance
Improve network performance with tremendous degree of monitoring, communication, collaboration, project management and high-fidelity data management.
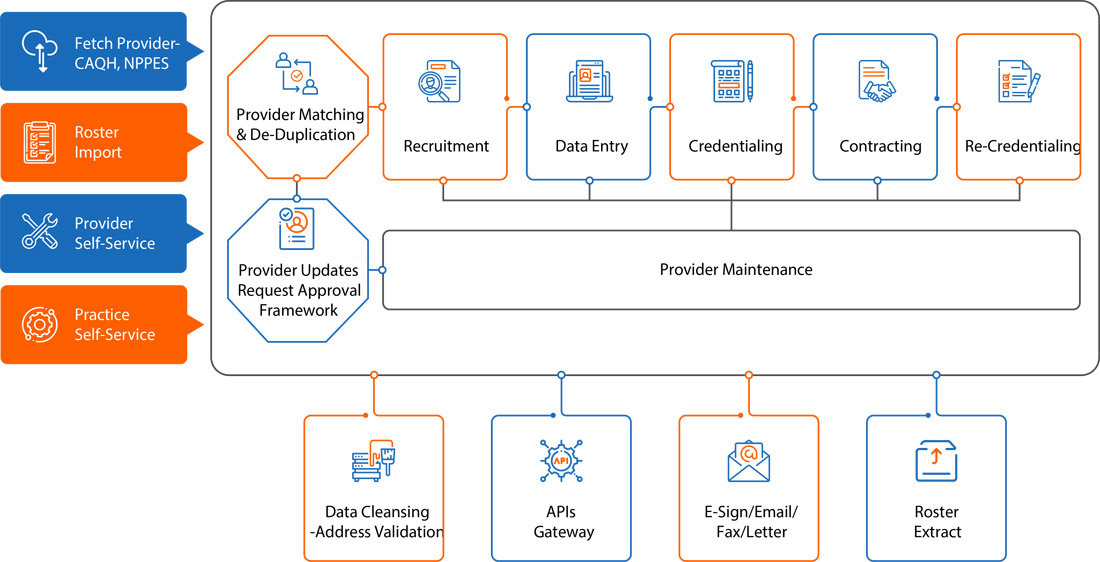
I-Network - An enterprise application with interoperability
Highly acclaimed technology-based solution that enables health plans and their network management teams to more effectively manage their provider networks. Utilizing I-Network, health plans can have confidence that their networks are doing what they need to, faster and more accurately.
I-Network manages following sets of logistically and practically complicated activities:-
 Improve member experience & Net Promoter Score (NPS)
Improve member experience & Net Promoter Score (NPS) Improve Provider experience and satisfaction
Improve Provider experience and satisfaction Maximize Compliance
Maximize Compliance Require Fewer, Less Complex Operations
Require Fewer, Less Complex Operations







